Due in large part to the pandemic, telemedicine is here to stay. This is good news, as having telemedicine system components that allow remote doctor/patient consultations and visits has provided more access to healthcare as well as making it quicker and more convenient than a trip to the nearest hospital.
The telehealth and telemedicine market reached $214.55 billion in 2023 and is projected to grow to $869.22 billion by 2033, with a CAGR of 15.5%. Notably, cloud-based delivery models hold 67% of the market, and telemedicine platforms boast a significant 45% market share.
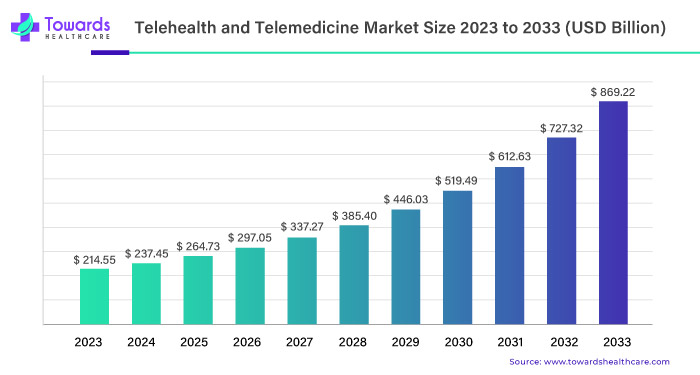
The steady market growth proves that telemedicine is here to stay. This is good news, as having telemedicine system components that allow remote doctor/patient consultations and visits has provided more access to healthcare as well as making it quicker and more convenient than a trip to the nearest hospital.
Telemedicine systems offer significant benefits for businesses, including reduced operational costs, increased efficiency, and expanded reach to rural or underserved areas. By integrating telemedicine solutions, healthcare providers can optimize resources, improve patient satisfaction, and enhance care delivery.However, you must consider lots of factors to build a secure, reliable, and user-friendly telemedicine system architecture. It involves robust cybersecurity, seamless communication interfaces, intuitive user experiences for patients and providers, and ensuring regulatory compliance and system interoperability for successful telemedicine implementation.
In this article, we’ll describe how a system operates and the major components of telemedicine solution architecture, along with challenges in developing and implementing it in a hospital or healthcare network.
What is Telemedicine?
Telemedicine is generally defined as the system of networks, software, and computers that allow a patient to schedule an appointment and have video and/or audio consultation with a health practitioner.
The practitioner should be able to use the system to order any necessary prescriptions as well as access the patient’s electronic health records and document/record the visit.
The doctor or nurse should also have the ability to be able to refer the patient to a specialist, if necessary, transferring all the necessary information.
Security and transparency is also a very important part of the telemedicine system architecture.
By law, patient medical records must be private and protected from hackers; doctors and nurses that use it should be verified as being licensed by the state.
Additionally, if things go wrong, such as a no-show from the patient or doctor, the appropriate steps need to be taken to prevent the insurer from being billed for something that didn’t occur.
It’s best if emergency systems are also integrated into telemedicine platform architecture, so that if the practitioner needs to call an ambulance, they can quickly alert a public or private service that is in the patient’s vicinity and take them to the hospital.
Certain situations also require telementoring, which is the ability for another doctor or specialist to be alerted and connected so they can further assist with diagnosis or monitoring outcomes.
Telemedicine Platform Architecture
Designing a sophisticated platform requires a comprehensive approach to integrating advanced technologies for seamless operation across healthcare scenarios. Below, we explore the technical components of telemedicine and considerations crucial for building a robust system.
Hardware Integration
Hardware is one of essential telemedicine components. It extends beyond basic cameras and microphones, encompassing advanced medical devices and sensors capable of real-time health data monitoring. These devices, often IoT-enabled, facilitate continuous monitoring of vital signs such as ECG, blood pressure, and oxygen saturation.
Integration with Electronic Medical Devices (EMDs) enables accurate data transmission, helping healthcare providers to make informed decisions remotely.
Secure Data Infrastructure
Secure data centers equipped with high-capacity servers and databases are the backbone of telemedicine architecture. Alternatively, cloud-based solutions can be used to provide scalable storage and computing power while adhering to stringent healthcare data protection standards (e.g., HIPAA).
Advanced encryption protocols and multi-factor authentication are required for data integrity and confidentiality during transmission and storage. Adhering to these security standards helps safeguard sensitive patient information from cyber threats.
Smart Scheduling and Workflow Automation
Scheduling is one of the core components of telemedicine system. Telehealth platforms utilize AI-driven scheduling algorithms that consider healthcare provider availability, patient preferences, and clinical urgency to minimize wait times and streamline virtual consultations.
Intelligent scheduling systems create an appointment and then block out the appropriate time frame to prevent double booking. If an appointment is canceled, advanced systems can fill the vacant time with a waiting list. It optimizes resource allocation and boosts profitability.
Workflow automation helps make the hospital as efficient as possible. Automated workflows seamlessly integrate with Electronic Health Records (EHR) and Practice Management Systems (PMS). It enables seamless data exchange and enhances clinical decision-making through comprehensive patient insights.
This way, the patient can connect with the correct practitioner at the correct time, who will have access to all the information they need.

Telepresence and Virtual Collaboration
Enhancing telepresence involves the integration of immersive technologies such as augmented reality (AR) and virtual reality (VR) to simulate in-person interactions between patients and providers. AR-enabled tools provide anatomical overlays and procedural guidance during remote examinations, enhancing diagnostic accuracy and patient engagement.
Virtual collaboration platforms enable multidisciplinary care teams to collaborate in real time. It fosters efficient communication and shared decision-making across geographical boundaries. Ultimately, these components of telehealth enable the patient and doctor to have almost the same experience as if they were in the same room together.
User Experience
User-centric design principles in telemedicine system architecture drive the development of intuitive telemedicine interfaces accessible via web browsers and mobile applications. Customizable dashboards empower healthcare providers to personalize workflows and access patient data seamlessly.
Patient portals offer secure communication channels, appointment scheduling, and teleconsultation histories, promoting patient engagement and adherence to treatment plans.
The Core Components of Telemedicine: Enhancing Patient Care
What are the three components of telemedicine? Communication technologies, data management systems, and remote monitoring devices are the top three elements for enhancing patient care and outcomes. These components of telemedicine system form a cohesive framework that supports efficient communication, secure data management, and streamlined healthcare delivery processes.
Communication Infrastructure
Effective telemedicine solutions rely on communication infrastructure to facilitate seamless interactions between patients and healthcare providers. These components of telehealth include video conferencing systems with high-definition cameras and audio equipment for clear, real-time communication during teleconsultations and other support channels.
Messaging platforms integrated into telemedicine platform architecture enable asynchronous communication for non-urgent queries and follow-ups. Integrating telephony systems allows for direct communication channels, improving accessibility and responsiveness in delivering remote healthcare services.
Patient support is one of the critical components of a telemedicine system communication technology. A telemedicine solution should integrate dedicated patient support channels like chat, email, or phone. Integrating chatbots helps interact with patients in real time, provide initial triage, answer FAQs, schedule appointments, and direct users to appropriate resources or healthcare providers based on their queries and needs.
Data Management Systems
Implementation of advanced data management systems is central to telemedicine system architecture. These systems securely manage patient health information, enabling the capture and retrieval of comprehensive patient records remotely. Cloud-based storage solutions provide scalable infrastructure for storing medical data while adhering to stringent data protection regulations.
Advanced encryption protocols and data backup mechanisms safeguard sensitive information, ensuring patient confidentiality and compliance with healthcare privacy laws.
Remote Monitoring Devices
Telemedicine architecture should allow for the integration of remote monitoring devices and wearable technologies. These devices collect real-time physiological data such as heart rate, blood pressure, and glucose levels, providing clinicians with actionable insights for remote patient management. It enables continuous health monitoring outside traditional clinical settings.
Connected to telemedicine platforms, these devices support proactive health management, early detection of health issues, and personalized treatment adjustments, enhancing patient autonomy and healthcare outcomes.

Building a Telemedicine Platform
Creating a system from scratch is challenging and expensive, especially doing it in-house. And trying to roll out all components at once can be a very heavy lift for both IT and staff.
One of the best solutions is to begin by using a modified version of existing conferencing software which can create a solid base from which to expand.
At S-PRO, we’ve done quite a bit of research into video conferencing software, some of which we include below.
Google Hangouts and Skype
We do not recommend either of these popular platforms as they do not have an API, which means they can’t be integrated into your website or system.
Zoom
This is our number one choice, as it only requires about 30-40 hours on the backend.
While it doesn’t work with Safari, it is commonplace enough that a lot of people are familiar with it and can use the app; it also has a good SDK and Rest-api for application integration.
However, since storage on Zoom is expensive, we usually recommend downloading the videos and saving on your own server.
AWS Chime
This is a good second choice as it requires just 25-30 hours for the backend and 10 for DevOps, for a total of 40 hours.
It can also be integrated to your website using SDK, or you can use the web or phone application.
It has all the features of Google Hangouts and good documentation; however, it is more expensive than Zoom.
Cisco WebEx
As a third option, Cisco’s WebEx is very similar to Zoom in terms of pricing and capabilities, but takes slightly longer to integrate; this is largely due to poor documentation.
It also doesn’t have a direct link to the conference, instead putting users in a “waiting room”; however this could also be seen as more akin to a real visit to the doctor’s office.
On the plus side, you can keep up to 10 gb of video in the cloud.
Summary
Telemedicine is the “new normal” in digital health.
Telemedicine systems can be quite complex, giving patients and practitioners an experience that is the next best thing to a physical visit.
For hospitals and facilities looking to upgrade their systems, it’s best to start with video conferencing and expand from there.
At S-PRO, we are very experienced in configuring and building telemedicine systems.
We can advise you on the components you need as well as get you up and running in a very short amount of time.
If you’re interested, contact a representative today.





